Welcome to Fox Valley Memory Project
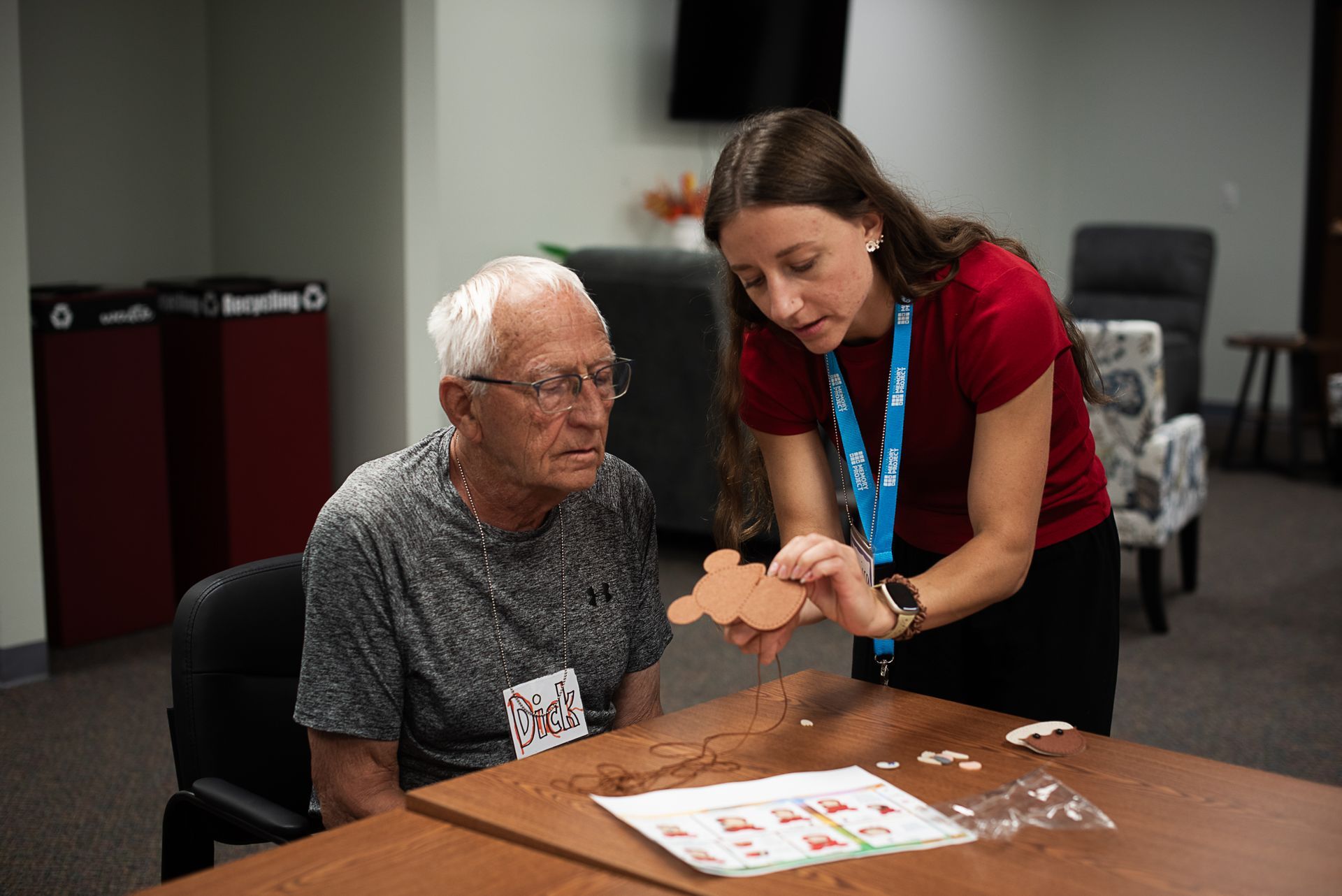
Fox Valley Memory Project supports individuals living with dementia and their care partners through engaging programs, educational resources, and meaningful social opportunities.
Our mission is rooted in the belief that everyone deserves to live with dignity, purpose and joy.
Whether you're seeking support, looking to connect with others, or simply exploring ways to live well with dementia, we are here to walk alongside you.
We Can Help
We strive to serve our whole community, providing resources for care partners, families, and anyone looking to learn more!
Get Social
Our goal is to live well, so learn how we’re staying active with monthly programs, memory cafes and social events!
Newsletter
Learn what's new, get the latest information on our popular newsletter. All the info you need in one place.
Invest in FVMP
Learn more about how you can volunteer your time or make a contribution to our organization.
Who We Serve
Individuals with Dementia
Care Partners
Family & Friends
Area Businesses & Organizations
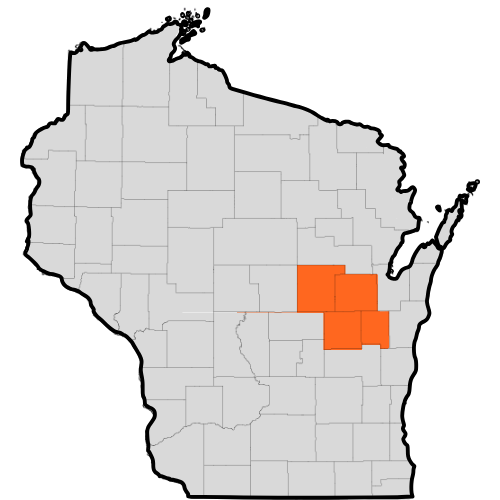
Our Service Areas
Calumet, Outagamie, Waupaca, and Winnebago counties